Ileostomy
Introduction
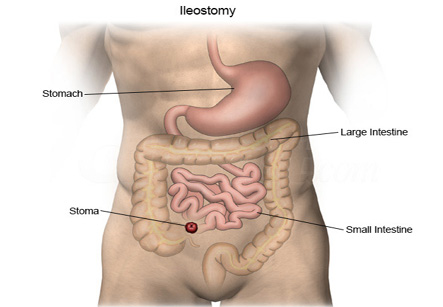
An ileostomy is a surgical procedure in which the small intestine is attached to the abdominal wall for bypassing the large intestine. Thus, the digestive waste exits the body through an artificial opening called as stoma (from the Greek word for “mouth”).
An ileostomy creates a temporary or permanent opening between the ileum (the portion of the small intestine which empties to the large intestine) and the abdominal wall. The colon or rectum may be removed or bypassed. A temporary ileostomy is recommended for patients undergoing bowel surgery (e.g., removal of a segment of bowel), to provide sufficient time for the intestines to heal without the stress of normal digestion.
The quality of life is usually not affected by an ileostomy. With proper care, most patients can avoid major medical complications.
Chronic ulcerative colitis is a medical condition which is treated with the removal of the large intestine. Ulcerative colitis occurs when the body’s immune system attacks the cells in the lining of the large intestine, which causes inflammation and tissue damage. An ileostomy is a suitable treatment for patients who do not respond to medical or dietary therapies in ulcerative colitis.
Other conditions which can be treated with an ileostomy include:
• Bowel obstructions
• Colon or rectal cancer
• Crohn’s disease (chronic inflammation of the intestine)
• Congenital bowel defects
• Severe bleeding from the large intestine
• Injury to the intestinal tract
Procedure:
For some patients, an ileostomy is preceded by removal of the colon or both the colon and rectum (proctocolectomy). Patient is given general anesthesia. An incision is made down the patient’s midline, through the abdominal skin, muscle, and other subcutaneous tissues. Once the abdominal cavity is opened, the colon and rectum are isolated and removed. The anal canal is stitched and closed.
Other patients undergoing ileostomy have only a temporary bypass of the colon and rectum. This includes patients undergoing small bowel resection or the creation of an ileo-anal anastomosis . In ileoanal anastomosis, the surgeon makes a pouch of tissue from the ileum and connects it directly to the anal canal.
There are two basic types of permanent ileostomy: conventional and continent
A conventional ileostomy
This is also called as Brooke ileostomy, which involves a separate, smaller incision through the abdominal skin (usually on the lower right side) to which the cut end of the ileum is sutured. The ileum may slightly protrude from the skin, often as far as 2 in (5 cm). Patients with this type of stoma are considered fecal-incontinent. This means that they can no longer control the emptying of wastes from the body. After a conventional ileostomy, the patient is fitted with a plastic bag over the stoma and attached to the abdominal wall skin with adhesive. The ileostomy bag collects waste exiting from the body.
A continent ileostomy
It is also called as a Kock ileostomy. This procedure allows a patient to control when waste should exit the stoma. Portions of the small intestine are used to form a pouch and valve. These are then directly attached to the abdominal wall skin to form a stoma. Waste collects in the pouch and can be expelled by insertion of a soft, flexible tube through the stoma any time of the day.
Preparation
The patient meets with the operating surgeon before surgery to discuss the details of the surgery and receive instructions on pre- and post-operative care. Just before the surgery, an intravenous (IV) line is placed for administering fluid and medications. The patient is given a bowel prep to cleanse the bowel and prepare it for surgery. The location where the stoma will be placed is marked, away from bones, abdominal folds, and scars.
Aftercare
Following surgery, the patient is instructed about the care of the stoma, placement of the ileostomy bag, and changes to diet and lifestyle. As the large intestine is no longer a part of the digestive system, fecal matter exiting the stoma has high water content. The patient must therefore increase the fluid intake to minimize the risk of dehydration. Visits with an enterostomal therapist or a support groups may be recommended to help the patient adjust to living with a stoma. After the ileostomy heals, a normal diet can usually be resumed, and the patient can also return to normal activities.
Risks
Risks associated with the ileostomy procedure include:
1. Severe bleeding
2. Infection
3. Complications due to general anesthesia
Risks after the surgery:
1. Stomal obstruction (blockage)
2. Inflammation of the ileum
3. Stomal prolapse (protrusion of the out of the stoma)
4. Irritation of the skin around the stoma.
Results:
The quality of life is usually not affected by an ileostomy. With proper care, most patients can avoid major medical complications. However, patients with a permanent ileostomy may suffer from emotional problems and benefit from psychotherapy.